The immune system is a vast network that spans the entire length of the body. From our protective skin barrier to our gut microbiome, our immune system is always on high alert as it attempts to keep foreign objects, like viruses and harmful bacteria, from infecting the body. It’s an uphill battle for the immune system, though, as it also contends with factors like diet and stress. One way to potentially balance the immune system and bring the body back to equilibrium is through the application of prebiotics and probiotics.
GUT MICROBIOTA
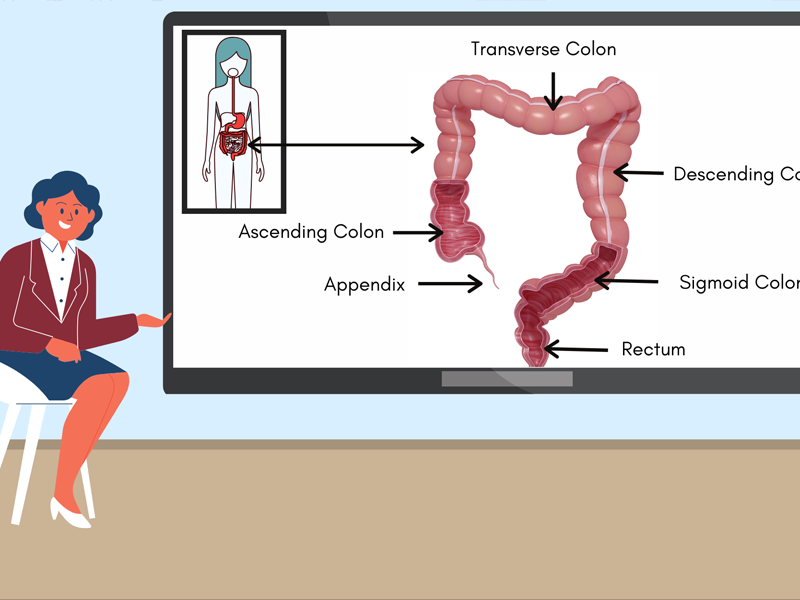
The gut microbiota consists of trillions of microorganisms. Collectively these bacteria, viruses, protozoans, and fungi, live in the human digestive system- specifically the colon. The beneficial bacteria, far from being simple passengers in the body, play an essential role in the body. These helpful bacteria break fibers down into the fuel for gut cells, help synthesize vitamins, and take space away from the “harmful” bacteria (1). They also play a crucial role in the immune system by triggering immune responses and by maintaining the integrity of the gut barrier. This important barrier allows nutrients into the bloodstream while also keeping out harmful bacteria, viruses, and toxins. (2)
HEALTHY, BALANCED GUT MICROBIOTA
When the gut microbiota is flourishing, with many different species of beneficial microbes, it provides up to 70% of immune system functions. (3)
HOW?
The “good” species of microbes feed on the fibers (4,5), soluble and insoluble, that the body cannot digest. Short Chain Fatty Acids, like acetic, propionic, and butyrate, are created as a byproduct. (6) Part of these SCFAs, specifically butyrate, are used to maintain the cells that make up the gut barrier. (7) The remaining SCFAs trigger cells in the gut barrier, leading to a cascade of cellular processes that ultimately activate T Cells. (8) T Cells specialize in defeating one particular type of antigen. They also signal macrophages, a more generalized pathogen killer, for backup. (9)
Additionally, just by taking up space and resources in the gut, these beneficial bacteria constrict the growth of more harmful strains of bacteria.
“GUT DYSBIOSIS” – DAMAGED GUT MICROBIOTA
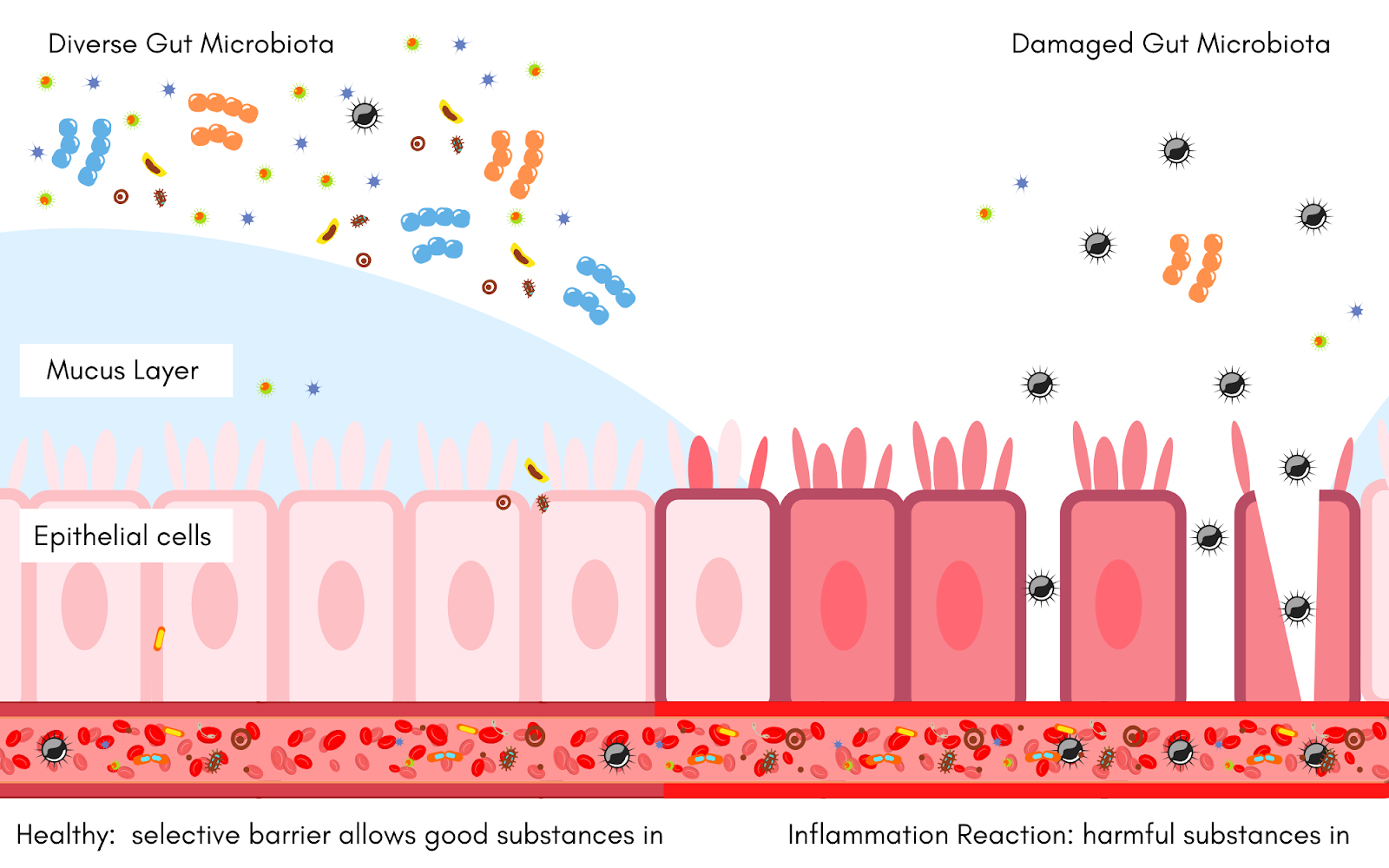
In a damaged gut microbiota, there is much less diversity of beneficial bacteria. Thus, processes that keep the gut barrier healthy and intake are not taking place as frequently. Without beneficial bacteria and subsequent SCFAs, the gut barrier loses its integrity. If it is not repaired, gaps or leaks appear in the gut barrier allowing harmful antigens to invade the bloodstream (10). An inflammatory response is triggered by this damage and the body reacts by sending C-Reactive Protein, a now known marker of inflammation to the site. Subsequently, harmful bacteria in the gut will take away valuable resources from the remaining beneficial bacteria and cause more inflammation. This creates a vicious cycle that further damages the gut and impairs the immune system response. (6) Breaking this cycle is imperative, as chronic inflammation can lead to obesity, food allergies, and even syndromes like Irritable Bowel Syndrome (IBS) (11) and Chronic Kidney Disease (CKD) (12)
.
EVERYDAY IMMUNE SYSTEM STRESSORS

The human immune system is under constant stress. It needs to contend with viruses, fungi, and harmful bacteria while also dealing with outside factors.
DIET
A diet low in fiber and high in sugar, fats, and refined carbohydrates have detrimental effects on the diversity of the gut microbiota. Without a steady stream of fiber, beneficial bacteria are unable to produce the energy the gut wall needs to repair itself. They are also unable to provide the necessary stimulus to the immune system. The immune system takes a further hit, as the harmful bacteria spread, feeding off the sugar, fats, and refined carbs. (13) Inflammation generally occurs as a result.
STRESS, ANXIETY, AND DEPRESSION
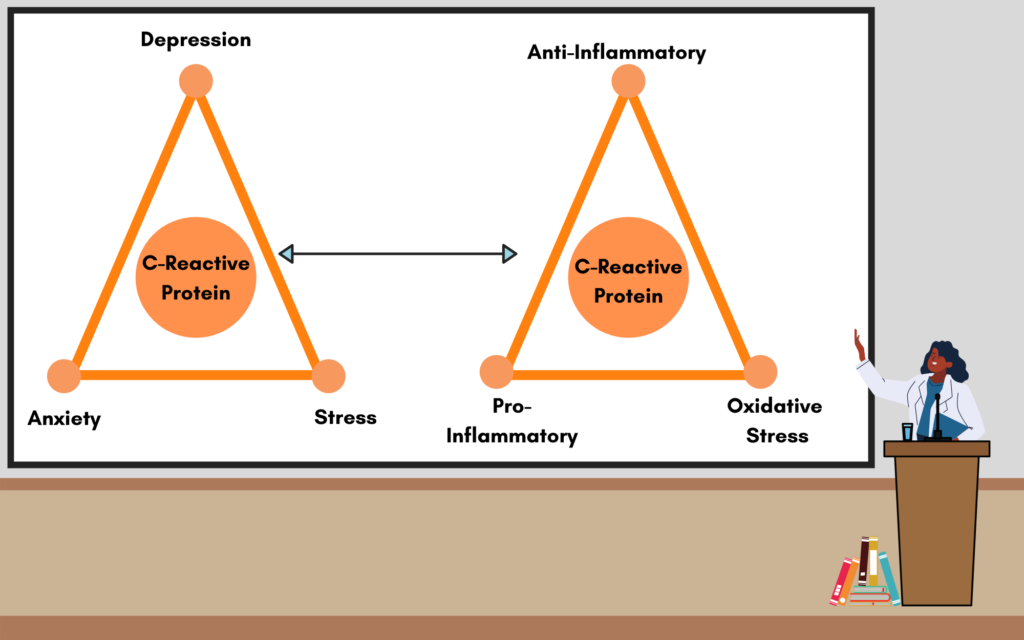
In the modern era, there are fewer things to run from but there are plenty of things to be stressed about. Regardless of stimulus, like a tiger or an angry boss, the body immediately releases hormones and consumes extra energy to prepare for the upcoming events. (14)
This reaction, with its many benefits, is not without consequence. The chemicals produced disrupt the bacteria, causing physical symptoms like stomach aches and nausea. Overall, chronic stress, anxiety, and depression affects appetite and digestion, interrupting the exchange of nutrients to the good bacteria, and then limiting how much fuel the gut barrier receives. (15) Ultimately, this may result in inflammation, marked by the presence of C-Reactive Protein.
MEDICATIONS AND ANTIBIOTICS
Medications, whether over the counter or prescribed by a doctor, and antibiotics may alter the composition of the gut microbiome. Many drugs and antibiotics target inflammation and ultimately reduce the amount of C-Reactive Protein. However, there is significant evidence that many medications (and all antibiotics) affect the growth of at least one species or two species in the gut. But, because each human has an incredibly unique array of bacteria, it is hard to predict which species will be affected. (16)
BRINGING THE BODY BACK TO EQUILIBRIUM
The gut cannot properly assist the immune system without the presence of a healthy gut microbiota filled with a diverse amount of beneficial bacteria. Despite the challenges modern humans face in maintaining their microbiota, there is a simple way to help bring the immune system back up to speed.
PROBIOTICS
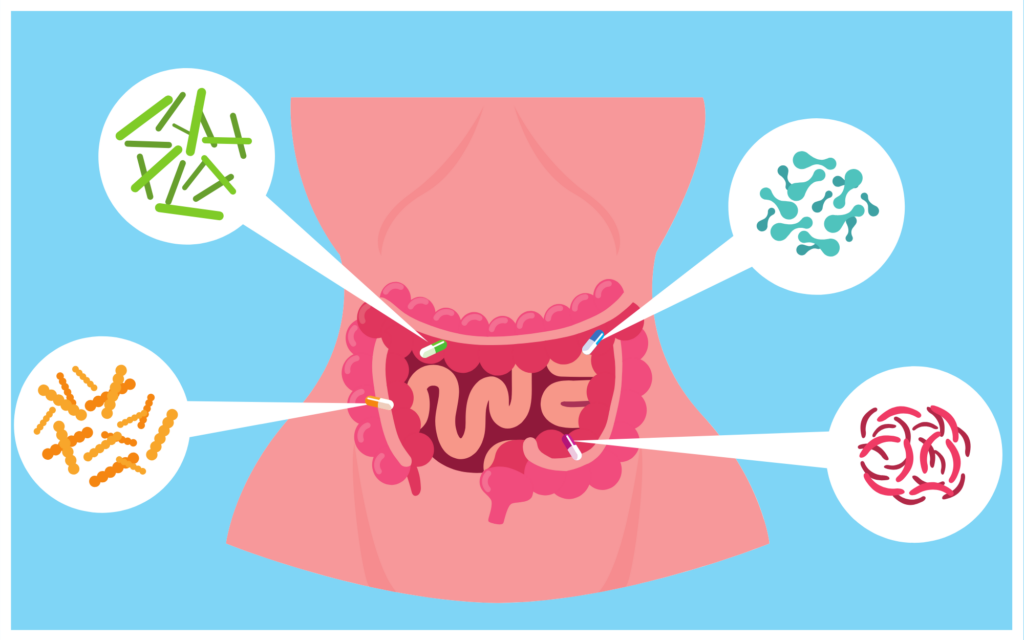
Probiotics are packaged, live beneficial bacteria that when taken in enough quantities may benefit the host. (17) Probiotics can replenish the body’s good bacteria, increasing the amount of energy the gut barrier receives and jumpstarting the crosstalk that activates the immune system. (7) Supporting the population of beneficial bacteria through the use of a highly studied, multi-strain probiotic supplement is an easy way to help repair the gut microbiome and restore the essential processes needed to reduce inflammation and C-Reactive Protein.
When looking for a probiotic, consider a multi-strain with high Colony Forming Units (CFUs) which indicates the amount of the probiotic bacteria present in the product. High amounts of CFUs help the bacteria establish themselves in the gut. Additionally, each strain of beneficial bacteria has its own unique effect on the gut.
PREBIOTICS

Dietary fiber is the indigestible part of plant foods that can’t be broken down by any of our digestive enzymes. The daily average amount of fiber a person should get a day is 25 grams, but only around 5% of Americans reach this daily goal. (26) Increasing generic fiber, however, shouldn’t be the primary concern. Different fiber sources provide very different benefits to the gut microbiota.
Look for a multi-fiber (functional fiber) product with soluble and insoluble fiber. Most prebiotic supplements include only a soluble or insoluble fiber when they should have both. After all, both types provide different benefits. Soluble fibers dissolve in water and are ultimately turned into SCFAs. Insoluble fiber doesn’t dissolve in water but it does provide fuel for the gut microbiota and assist bowel movements. (27) This will help ensure that multiple functions in the gut are assisted.
Reaching the daily recommended levels of fiber, soluble and insoluble, can significantly benefit the beneficial bacteria in the gut microbiota, which in turn lowers inflammation and benefits the gut barrier and immune response!
THE TAKE-AWAY
Maintaining a healthy gut microbiome and reducing inflammation is an imperative part of sustaining a balanced immune system. Consider how you can overcome everyday immune stressors. Try controlling anxiety, watching your diet, and taking a prebiotic and probiotic. Your gut microbiota will thank you for the extra assistance from these supplements by helping the immune system stay on track.
Works Cited:
- Kiran, M. D., Gharat, P. D., Vakharia, M. D., & Ranganathan, N. D. (2019). Specific Probiotics for Chronic Kidney Disease: A Review. The Indian Practitioner, 72(2), 1–12. Retrieved from https://kibowbiotech.com/pdf/Specific-probiotics-for-CKD-Review-Feb-2019.pdf
- Groschwitz, K. R., & Hogan, S. P. (2009). Intestinal barrier function: molecular regulation and disease pathogenesis. The Journal of allergy and clinical immunology, 124(1), 3–22. https://doi.org/10.1016/j.jaci.2009.05.038
- Vighi, G., Marcucci, F., Sensi, L., Di Cara, G., & Frati, F. (2008). Allergy and the gastrointestinal system. Clinical and experimental immunology, 153 Suppl 1(Suppl 1), 3–6. https://doi.org/10.1111/j.1365-2249.2008.03713.x
- Zimmer, C. (2018, January 1). Fiber Is Good for You. Now Scientists May Know Why. Retrieved from https://www.nytimes.com/2018/01/01/science/food-fiber-microbiome-inflammation.html
- Cummings, J. H., & Engineer, A. (2018, June). Denis Burkitt and the origins of the dietary fibre hypothesis. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28583217
- Krishnan, Kiran. (2020, April 23) Common Dysfunctions of the Standard American Gut in Chronic Illness. Fullscript Webinar. https://www.youtube.com/watch?v=z_b34ev-FGM
- Venegas, D. P., Fuente, M. K. D. L., Landskron, G., González, M. J., Quera, R., Dijkstra, G., … Hermoso, M. A. (2019). Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Frontiers in Immunology, 10. doi: 10.3389/fimmu.2019.00277
- Maldonado Galdeano C, Cazorla S, I, Lemme Dumit J, M, Vélez E, Perdigón G: Beneficial Effects of Probiotic Consumption on the Immune System. Ann Nutr Metab 2019;74:115-124. doi: 10.1159/000496426
- Cavanagh, M. (n.d.). T-cell activation. Retrieved from https://www.immunology.org/public-information/bitesized-immunology/systems-and-processes/t-cell-activation
- Wells, J. M., Brummer, R. J., Derrien, M., Macdonald, T. T., Troost, F., Cani, P. D., … Garcia-Rodenas, C. L. (2017). Homeostasis of the gut barrier and potential biomarkers. American Journal of Physiology-Gastrointestinal and Liver Physiology, 312(3). doi: 10.1152/ajpgi.00048.2015
- Martín, R., Chamignon, C., Mhedbi-Hajri, N. et al. The potential probiotic Lactobacillus rhamnosus CNCM I-3690 strain protects the intestinal barrier by stimulating both mucus production and cytoprotective response. Sci Rep 9, 5398 (2019). https://doi.org/10.1038/s41598-019-41738-5
- Crépin T, Legendre M, Carron C, et al. Uraemia-induced immune senescence and clinical outcomes in chronic kidney disease patients. Nephrology, Dialysis, Transplantation : Official Publication of the European Dialysis and Transplant Association – European Renal Association. 2020 Apr;35(4):624-632. DOI: 10.1093/ndt/gfy276
- Singh, R.K., Chang, H., Yan, D. et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med 15, 73 (2017). https://doi.org/10.1186/s12967-017-1175-y
- Stress and the Gut Microbiome. (2020, May 1). Retrieved from https://kibowfortis.com/stress-and-the-gut-microbiome/
- Stress Effects on the Body. (2018). Retrieved from https://www.apa.org/helpcenter/stress/effects-gastrointestinal
- Walsh, J., Griffin, B. T., Clarke, G., & Hyland, N. P. (2018). Drug-gut microbiota interactions: implications for neuropharmacology. British Journal of Pharmacology, 175(24), 4415–4429. doi: 10.1111/bph.14366
- Hill, C., Guarner, F., Reid, G. et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11, 506–514 (2014). https://doi.org/10.1038/nrgastro.2014.66
- https://kibowbiotech.com/pdf/kibow_flora_data_sheet.pdf
- Cummings, J. H., & Engineer, A. (2018, June). Denis Burkitt and the origins of the dietary fibre hypothesis. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28583217
- Ducrotté, P., Sawant, P., & Jayanthi, V. (2012). Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World Journal of Gastroenterology, 4012–4018. doi: 10.3748/wjg.v18.i30.4012
- Jones, M., Chen, H., Ouyang, W., Metz, T., & Prakash, S. (2004). Microencapsulated Genetically Engineered Lactobacillus plantarum 80 (pCBH1) for Bile Acid Deconjugation and Its Implication in Lowering Cholesterol. Journal of Biomedicine & Biotechnology. doi: 10.1155/S1110724304307011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC545656/
- Martín, R., Chamignon, C., Mhedbi-Hajri, N. et al. The potential probiotic Lactobacillus rhamnosus CNCM I-3690 strain protects the intestinal barrier by stimulating both mucus production and cytoprotective response. Sci Rep 9, 5398 (2019). https://doi.org/10.1038/s41598-019-41738-5
- Lactobacillus Acidophilus . (n.d.). Retrieved from https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=19&contentid=Lactobacillus
- Singh, A., Hacini-Rachinel, F., Gosoniu, M. et al. Immune-modulatory effect of probiotic Bifidobacterium lactis NCC2818 in individuals suffering from seasonal allergic rhinitis to grass pollen: an exploratory, randomized, placebo-controlled clinical trial. Eur J Clin Nutr 67, 161–167 (2013). https://doi.org/10.1038/ejcn.2012.197
- Olga A Zelenaia, Ph.D., Beena G Patel, Ph.D., Rahul S Dheer, B.S., Natarajan Ranganathan, Ph.D. Kibow Biotech Inc., Philadelphia, PA, United States of America. Journal of the American Society of Nephrology 14: Nov 2003 pp. 765A SU-PO1045. https://kibowbiotech.com/streptococcus-thermophilus/
- Quagliani, D., & Felt-Gunderson, P. (2017). Closing America’s Fiber Intake Gap: Communication Strategies From a Food and Fiber Summit. American Journal of Lifestyle Medicine, 11(1), 80–85. https://doi.org/10.1177/1559827615588079
- What is Dietary Fiber and How Can You Get Enough of It? (2020, May 1). Retrieved from https://kibowfortis.com/what-is-dietary-fiber/
- The Fiber Supplement You Never Knew You Needed. (2020, March 19). Retrieved from https://kibowfortis.com/the-fiber-supplement-you-never-knew-you-needed/
- Kibow Fortis®. (2019, September 10). Retrieved from https://kibowbiotech.com/kibow-fortis/